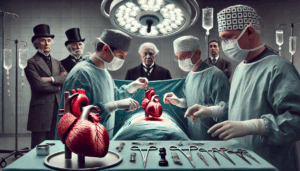
Minimally Invasive vs Conventional Coronary Bypass Surgery for Multivessel Coronary Disease
This study compared minimally invasive coronary surgery (MICS-CABG) to traditional sternotomy-based CABG in patients with multivessel coronary artery disease. Analyzing matched cohorts of 244 patients each, the research found similar completeness of revascularization and comparable 5-year major adverse cardiac and cerebrovascular events (MACCE). MICS-CABG also had high graft patency (96.2%) and fewer transfusion needs, indicating it as a viable surgical alternative.