Assistance from a Mixing Zone Model to Perform Aortic Femoral Perfusion Strategy with Severe Atherosclerotic and Artheromic Aortic Disease for Endoscopic Minimally Invasive Redo Mitral Valve Repair
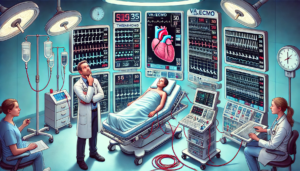
This study explores a novel perfusion strategy for minimally invasive redo mitral valve surgery in patients with severe atherosclerotic and artheromic aortic disease. Using a combination of antegrade and retrograde perfusion, the study evaluates the mixing zone during cardiopulmonary bypass (CPB) to optimize outcomes. A case study demonstrates the effectiveness of this approach, with no postoperative cerebral complications. Findings suggest that adjusting cannulation sizes can improve perfusion safety.