Background: Acute type A aortic dissection necessitates rapid and effective arterial cannulation techniques for optimal outcomes. This meta-analysis compares the safety and effectiveness of direct aortic cannulation (AoC) with peripheral cannulation (PC) via the femoral or axillary arteries in aortic surgery for acute type A aortic dissection.
Methods: A systematic review following PRISMA guidelines identified 10 retrospective studies encompassing 2518 patients (961 AoC, 1557 PC). Pooled odds ratios (OR) with 95% confidence intervals (CI) were calculated to analyze perioperative characteristics, short-term mortality rates, and postoperative complications including stroke and acute kidney injury.
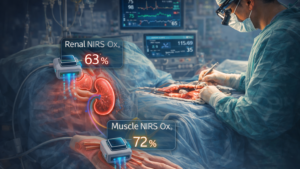
Results: Short-term mortality did not significantly differ between AoC and PC (OR [95% CI] = 0.78 [0.61-1.01], p = .06). Likewise, postoperative stroke (OR [95% CI] = 0.86 [0.63-1.17], p = .33) nor acute kidney injury (OR [95% CI] = 1.11 [0.89-1.37], p = .35) showed no significant differences. AoC exhibited shorter operation time whereas there were no significant differences in aortic cross clamp time and cardiopulmonary bypass time between both groups. Our meta-regression analysis, considering the distal extent of aortic replacement, indicated that variations in aortic replacement rates did not significantly impact the observed outcomes.
Conclusion: AoC is a viable alternative to PC for acute type A aortic dissection. While both approaches offer comparable outcomes, AoC’s advantage in shorter operation time warrants thoughtful consideration in clinical practice.
Keywords: acute aortic dissection; aortic cannulation; peripheral cannulation; surgical technique.