Evolution of Distal Limb Perfusion Management in Adult Peripheral Venoarterial Extracorporeal Membrane Oxygenation with Femoral Artery Cannulation
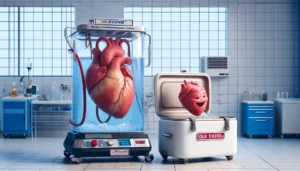
This narrative review explores the advancements in managing distal limb perfusion in venoarterial extracorporeal membrane oxygenation (VA ECMO) with femoral artery cannulation. Initially, no specialized techniques like distal perfusion cannulae were used, leading to limb ischemia. Recent innovations include prophylactic measures, various cannulation methods, and improved venous drainage techniques to enhance limb perfusion and reduce ischemic complications. Advanced monitoring tools like near-infrared spectroscopy aid in decision-making and management.