Brain Death Donors on Extracorporeal Membrane Oxygenation Support
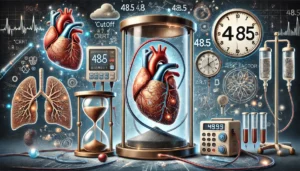
This study examines 15 brain death donors on extracorporeal membrane oxygenation (ECMO) support, admitted to a specialized intensive care unit between 2018 and 2023. The study evaluates the effect of a strict hemodynamic monitoring schedule during a 6-hour observation period on the utilization rate of organs. Results show an increase in utilization rates from 78% to 88% with no significant differences in donor characteristics or hemodynamic data between periods. Most donors required multiple vasoactive drugs to maintain adequate perfusion.