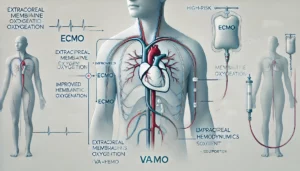
Fluid Management in Adult Patients Undergoing Venoarterial Extracorporeal Membrane Oxygenation: A Scoping Review
This review explores fluid management in patients supported by venoarterial extracorporeal membrane oxygenation (VA-ECMO). It highlights the lack of evidence for optimal fluid strategies, comparing liberal vs. restrictive approaches, or types like crystalloids and albumin. Fluid overload negatively affects survival and kidney outcomes, emphasizing the need for precise strategies. The study calls for rigorous research to determine effective fluid resuscitation approaches and improve clinical outcomes.